bodies recovered from water

The drowned (Wassilij Perow 1867)
Source: Wikipedia
Not every individual, whose body is recovered from water, has drowned.
When a body is recovered from water, the significant issues raised are frequently:
- Is the estimated post mortem interval consistent with witness evidence?
- Is there any pathological evidence to indicate cause of death?
- Is there any pathological evidence of natural disease, ante mortem injury or assault capable of providing an explanation for how the deceased came to find himself/ herself in, or fail to remove himself/ herself from, the water?
An additional problem for those investigating the deaths of those recovered from water is identification; frequently a body recovered from water is not capable of being identified by visual means, and other forms, such as dental or DNA identification will be required.
the forensic pathological approach to bodies recovered from water - the big picture
post mortem interval
Estimation of post mortem interval in water is unreliable (Giertsen 2000), but temperature is likely to be the most important factor governing decompositional changes.
There may be signs of immersion (wrinkling of the skin of the palms and soles; loosening of the skin, hair or nails); Polson and Gee (1973) state that maceration of the (exposed) hands and feet is likely to become ‘well established’ during the first week, showing signs of separation of the skin of the digits towards the end of that week. Detachment of skin becomes likely in the second week.
As a matter of interest, research into the process(es) underlying wrinkling of the skin of the fingers following immersion in water in life have hypothesised that water permeates sweat ducts and alters the electrolyte composition, following which autonomic nerve fibres in the digits are triggered. These mediate vasoconstriction, resulting in negative digit pulp pressure (Wilder-Smith and Chow 2002 and 2003).
The epidermis of the digit skin is firmly anchored to the deep dermis via epidermal ridges, which insert every 1mm along longitudinal lines, and this anchoring - which allows us to firmly gripo objects - results in variations in skin tautness (maximal at anchorage sites). Resistance blood vessels in digits are distributed in an inhomogenous manner; large numbers of 'glomus organs/ bodies' are present, which lose volume through vasoconstriction and help create negative digit pulp pressure. A pressure gradient between deep and superficial structures induces a downward pull on the overlying skin. This downward pull is uneven, and leads to the wrinkling seen following immersion.
Little by little he distinguished the bodies, and went from one to the
other. It was only the drowned that interested him. When several human
forms were there, swollen and blued by the water, he looked at them
eagerly, seeking to recognise Camille. Frequently, the flesh on the
faces had gone away by strips, the bones had burst through the mellow
skins, the visages were like lumps of boned, boiled beef. Laurent
hesitated; he looked at the corpses, endeavouring to discover the lean
body of his victim. But all the drowned were stout. He saw enormous
stomachs, puffy thighs, and strong round arms. He did not know what to
do. He stood there shuddering before those greenish-looking rags, which
seemed like mocking him, with their horrible wrinkles.Therese Raquin. Emile Zola 1867
cause of death

After the storm (Slinkachu via the Telegraph)
(a) Evidence of drowning
Regardless of the composition of water/ fluid, ‘drowning’ (the ‘process of experiencing respiratory impairment from submersion in a liquid’ (van Beeck et al 2005)), may result in pulmonary surfactant insufficiency/ damage, pulmonary oedema, alveolitis, hypoxaemia, and metabolic acidosis (Modell 1993, Pearn 1985, Orlowski 1987).
Extensive experimental (animal) and clinical (human) data exist in the scientific literature, identifying differences between, for example, fresh water and seawater drowning; active respiration of fresh water results in alveolar collapse/ atelectasis, due to the alteration of the surface tension properties of pulmonary surfactant, resulting in intra-pulmonary shunts. Because it is hypotonic with respect to plasma, fresh water is rapidly absorbed into the bloodstream, causing transient (but clinically irrelevant) electrolyte dilution and hypervolaemia. Sea water causes surfactant loss, and because it is hypertonic with respect to plasma, results in fluid shifts into alveoli, plasma electrolyte hyperconcentration and hypovolaemia. (Modell 1993, Pearn 1985, Modell and Davis 1969, Modell et al 1966).
Fresh/ seawater aspiration leads to systemic hypoxaemia causing myocardial depression, reflex pulmonary vasoconstriction and altered pulmonary capillary permeability contributing to pulmonary oedema (Lunetta and Modell 2005).
Experimental evidence (Modell and Moya 1966, Modell et al 1967) shows that there is an inverse relationship between survival and the volume of aspirated fluid (sea water being twice as lethal as fresh water), but even small quantities (i.e. as little as 30 mL) caused arterial hypoxaemia.
Autopsy findings ascribed to drowning (‘external’ foam (i.e. visible at the mouth or nostrils), frothy fluid in the airways and lung ‘hyper-expansion’ reflect the pathophysiology of submersion and aspiration of the drowning medium; none of these, however, is diagnostic of drowning or present in all ‘verified’ drownings. (Lunetta and Modell 2005, Saukko and Knight (2004), Modell et al 1999).
In a series of 1590 bodies recovered from water, Lunetta et al (2002) found external foam in 29%, froth in the airways in 70.6% and overlapping of the lung margins in 64.1% of ‘fresh bodies’ of ‘verified drownings’; the combination of all three was present in only 8.8% of cases, but was said to be ‘100% specific for drowning’.
Suggested ‘signs of drowning’ reported in the literature include;
(i) External foam/ froth and frothy fluid in the airways reflects an admixture of bronchial secretion/ mucus, proteinacious material and pulmonary surfactant with the aspirated liquid (Lunetta et al 2002), which may persist for several days after death, and has been described as being ‘different in quality’ – more tenacious and persistent - from pulmonary oedema produced by other conditions (including cardiac failure, for example)(Modell et al 1999). Frothy secretions may be ‘washed away’ by flowing water during the submersion or recovery period, or may be absent due to the length of time spent immersed.
(ii) ‘Emphysema aquosum’ is the term used to describe hyperexpanded and ‘waterlogged’ lungs, whose medial margins ‘meet in the midline’, and which do not collapse on removal from the body. There may be ‘rib imprints’ on their pleural surfaces, and copious frothy fluid may exude from their cut surfaces (Giertsen 2000, Saukko and Knight 2004). See Magdeburg University's Virtual Pathology website for a 'pot specimen' of emphysema aquosum which can be rotated using your mouse wheel.
Combined lung weight of over 1Kg are comparable with ‘normal’ lung weights (de la Grandmaison et al 2001), but overlapping with that seen in fresh water drownings in Copeland’s series (Copeland 1985). However, Lunetta et al (2002) argue that lung weight alone is of ‘limited value’ for the diagnosis of drowning.
(iii) Pleural fluid accumulation. It has been stated (Morild 1995) that there is an association between drowning, post mortem submersion/ immersion interval and pleural fluid accumulation. However, data to the contrary has been presented by Yorulmaz et al (2003).
(iv) Sub-pleural haemorrhages (‘Paultauf’s spots’). These probably reflect haemolysis within intra-alveolar haemorrhages, and have been described in 5-60% of drownings (Lunetta and Modell 2005).
(v) Additional (morphological) ‘signs’ of drowning - ‘middle ear congestion and haemorrhage’, bloody/watery fluid in the sinuses and engorgement of solid organs, including the liver, reduction in the weight of the spleen, and muscular haemorrhages in the neck and back, are non-specific (Lunetta and Modell 2005).
(vi) Microscopy (particularly of the lungs) in the diagnosis of drowning has been described as yielding ‘nothing conclusive’(Giertsen 2000) and is ‘unreliable’ (Saukko and Knight 2004); there may be distension and/ or rupture of alveolar walls, alveolar haemorrhage and ‘narrowing of pulmonary capillaries’ (Lunetta and Modell 2005).
(vii) Diatom testing. Samples of major organs, and bone marrow, are often retained for diatom testing (eg. Kidney, liver, brain). The utility of such testing is ‘controversial’ (Peabody 1980); diatoms have been said to be ubiquitous in food and the environment, in non-drowning deaths, and absent in ‘known cases of drowning’. (Saukko and Knight 2004, Hendy 1973, Foged 1983).
(viii) Blood chloride content/ specific gravity analysis is considered to be ‘of no practical utility for the diagnosis (of drowning)’ (Lunetta and Modell 2005); analysis of blood strontium (Azaparren et al 1998) has also been suggested as a means with which drowning may be diagnosed.

Diatoms under the microscope
Source: Suspicious anatomy
(b) Evidence of an alternative mechanism(s)?
Drowning without evidence of liquid aspiration (‘dry drowning’) has been reported in up to 15% of cases, although in a series of 578 adults presumed to have drowned (Lunetta et al 2004), only 1.4% had lungs of ‘normal weight’ and no macroscopic signs of over-inflation.
Rather than represent true ‘drowning’, these deaths may be due to an alternative mechanism such as trauma, the effects of intoxication, arrhythmia, laryngospasm, or some other neurologically mediated mechanism (Modell et al 1999, Saukko and Knight 2004).
Stimulation of trigeminal nerve receptors by immersing the face (and laryngeal/ pharyngeal mucosa) in water has been shown to elicit reflex apnoea, bradycardia and peripheral vasoconstriction in humans- the so-called ‘diving response’ (Suzuki 1996, De Burgh Daly et al 1979), which is augmented by anxiety/ fear (Wolf 1966), a water temperature of less than 20 ºC (Pearn 1985) and, possibly, alcohol (Pearn 1984), increasing the likelihood of the development of a fatal arrhythmia. Cardiac arrest has also been documented following entry of water into the nose (Datta and Tipton 2006).
The ‘cold shock response’ - initiated by peripheral subcutaneous receptors - causes respiratory effects (inspiratory gasp and uncontrolled hyperventilation, respiratory alkalosis, cerebral hypoxia and possibly ventricular fibrillation) and cardiovascular effects (tachycardia, increased cardiac output, hypertension and ‘heart strain’, potentially leading to cardiac irritability and ventricular fibrillation), which appear temperature dependent (Tipton 1989, Datta and Tipton 2006). Co-stimulation of both diving and cold shock responses may precipitate supraventricular arrhthmias (Golden et al 1997).
why was the deceased in the water, and why could they not get out?
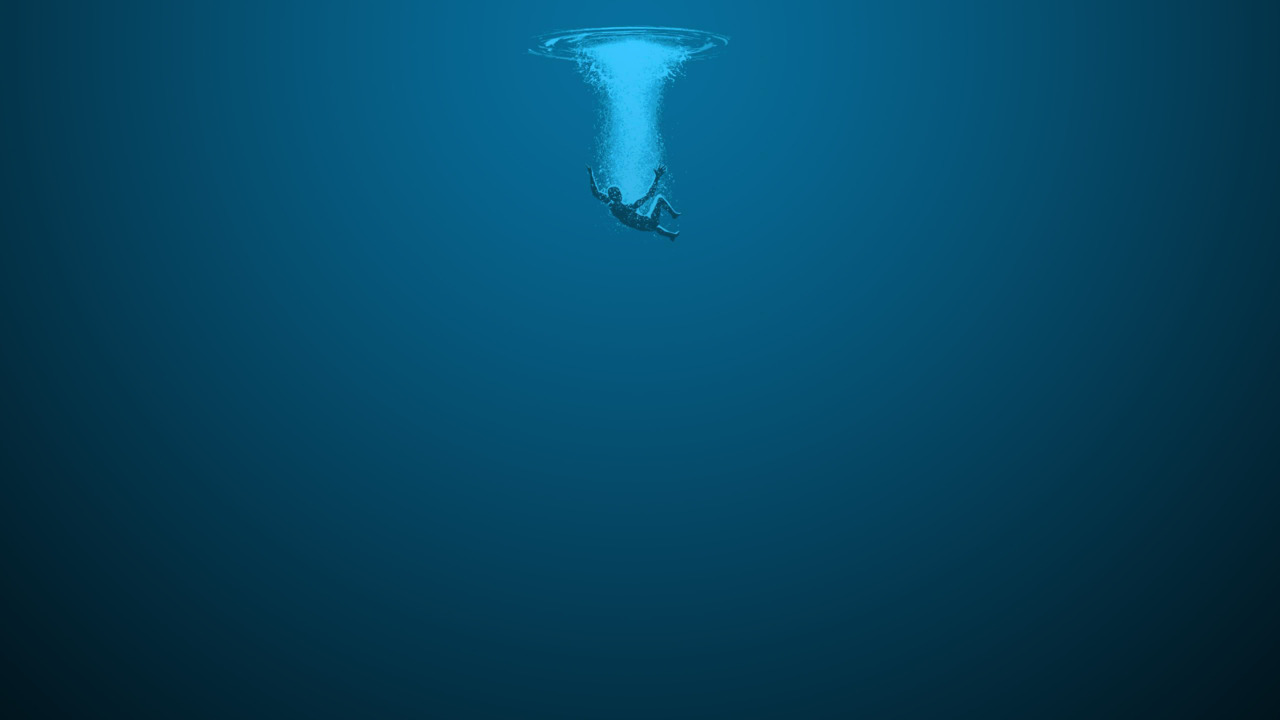
'Sinking feeling that I know all too well', Haley Kate via Tumblr
(a) Intoxication.
Despite evidence that alcohol is frequently found in the blood of adult drowning victims (Howland and Hingson 1988, Quan and Cummings 2003, Wintermute et al 1990), a causative role between alcohol and drowning has not been proven.
Lunetta et al (2004) found that the strongest association between drowning and alcohol was in relation to ‘fall-related’ cases (82.8%), and it is possible that an individual, whose body is recovered from water, came to be in the water because of an accidental fall due to alcohol intoxication. It is also an individual may have suffered a fatal alcohol-related concussive head injury, for example (Milovanovic and Di Maio 1999, Ramsay and Shkrum 1995).
Suicide by drowning is rare (and not usually associated with alcohol intoxication); reports in the literature estimate 4.5% (Copeland 1987) to 8.9% (Avis 1993) of all suicides.
(b) Natural disease.
Had the deceased any history of cardiovascular disease, or seizure disorder, capable of providing an explanation for falling into a body of water, or for their inability to get out of the water, following an arrhythmia/ seizure?
(c) Ante mortem injury/ assault.
The ‘vast majority of homicidal drownings’ involve forms of violence such as ‘beating’ and stabbing etc (Lunetta and Modell 2005). Careful evaluation of any injuries present is required in order to determine whether any could have been caused by assault during life. Injuries to the facial skeleton, neck (including larynx) or ulnar borders of the arms (suggestive of ‘defensive’ injuries), for example, should be excluded. It is not always possible, due to the effects of immersion, confidently to determine whether all or some of the injuries present are ante/ peri or post mortem in origin. Marine animals/ fish may cause skin, soft tissue or skeletal damage that may sometimes cause interpretation difficulties (Rutty 2001), and injuries caused by contact between the body and submerged objects, structures, rocks, gravel etc are frequently seen. In some bodies of water, damage may be caused by propeller blades, resulting in severe ‘chopping injuries’ and amputations.
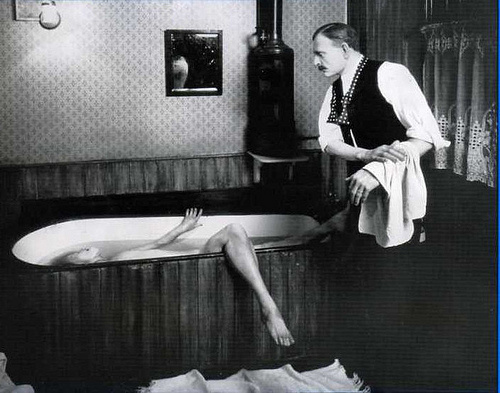
Madame Tussaud's model of George Joseph Smith - the Brides in the Bath murders
Homicidal 'death in the bath-tub'
cause/ manner of death
‘Classical’ anatomical signs of drowning are frequently absent, and this may be a reflection of post mortem interval; their absence does not exclude the diagnosis.
On the pathological/ toxicological findings alone, it is not always possible to be certain about the most likely cause of death in the case of a body recovered from water. A ‘diagnosis’ of drowning may be possible, but in some cases where a range of possibilities exist, it may be considered appropriate (Davison and Leadbeatter 1996) to give the medical cause of death as; 1a Indeterminate.
The manner of death is frequently accidental, but suicidal drowning has been described (Copeland 1987, Avis 1993), and disposal of bodies in water is well recognised following homicide (Copeland 1986).
references
- Avis SP. Suicidal drowning. Journal of Forensic Sciences 1993; 38: 1422-1426
- Azaparren JE, Vallejo G, Reyes E et al. Study of the diagnostic value of strontium, chloride, haemoglobin and diatoms in immersion cases. Forensic Science International 1998; 91: 123-132
- Copeland AR. An assessment of lung weights in drowning cases – the Metro Dade County experience from 1978 to 1982. The American Journal of Forensic Medicine and Pathology 1985; 6(4): 301-304
- Copeland AR. Homicidal drowning. Forensic Science International 1986; 31: 247-252
- Copeland AR. Suicide by drowning. The American Journal of Forensic Medicine and Pathology 1987; 8: 18-22
- Datta A, Tipton MJ. Respiratory responses to cold water immersion: neural pathways, interactions, and clinical consequences awake and asleep. Journal of Applied Physiology 2006; 100: 2057-2064
- Davison AM, Leadbeatter S. Confession of ignorance of causation in coroners’ necropsies – a common problem?. Journal of Clinical Pathology 1996; 49:439-443
- De Burgh Daly M, Angell-James JE, Elsner R. Role of carotid-body chemoreceptors and their reflex interactions in bradycardia and cardiac arrest. The Lancet 1979; 1(8119): 764-767
- de la Grandmaison GL, Clairand I, Durigon M. Organ weight in 684 adult autopsies: new tables for a Caucasoid population. Forensic Science International 2001; 119: 149-154
- Foged N. Diatoms and drowning – once more. Forensic Science International 1983; 21: 153-159
- Franks CM, Golden FS, Hampton IF, Tipton MJ. The effect of blood alcohol on the initial responses to cold water immersion in humans. European Journal of Applied Physiology and Occupational Physiology 1997; 75: 279-281
- Giertsen JC. ‘Drowning’, Chapter 16 In: ‘The pathology of trauma’, Mason JK, Purdue BN (Eds), 3rd Edition, Arnold Publishing 2000, London UK
- Golden F St C, Tipton MJ, Scott RC. Immersion, near-drowning and drowning. British Journal of Anaesthesia 1997; 79: 214-225
- Hendy NI. The diagnostic value of diatoms in cases of drowning. Medicine, Science and the Law 1973; 13: 23-34
- Howland J, Hingson R. Alcohol as a risk factor for drownings: a review of the literature (1950-1985). Accident Analysis and Prevention 1988; 20: 19-25
- Lunetta P, Penttila A, Sajantila A. Circumstances and macropathologic findings in 1590 consecutive cases of bodies found in water. The American Journal of Forensic Medicine and Pathology 2002; 23(4): 371-376
- Lunetta P, Modell JH, Sajantila A. What is the incidence and significance of ‘dry lungs’ in bodies found in water?. The American Journal of Forensic Medicine and Pathology 2004; 25: 291-301
- Lunetta P, Smith GS, Pentilla A, Sajantila A. Unintentional drowning in Finland 1970-2000: a population-based study. International Journal of Epidemiology 2004; 33: 1053-1063
- Lunetta P, Modell JH. Macroscopical, microscopical, and laboratory findings in drowning victims – A comprehensive review. Chapter 1. In: ‘Forensic Pathology Reviews – Volume 3’, Tsokos M (Ed), Humana Press 2005, Totowa USA
- Milovanovic AV, Di Maio VJM. Death due to concussion and alcohol. The American Journal of Forensic Medicine and Pathology 1999; 20: 6-9
- Modell JH, Gaub M, Moya F et al. Physiological effects of near drowning with chlorinated fesh water, distilled water and isotonic saline. Anesthesiology 1966; 27: 33-41
- Modell JH, Moya F. Effects of volume of aspirated fluid during chlorinated fresh water drowning. Anesthesiology 1966; 27: 662-672
- Modell JH, Moya F, Newby EJ et al. The effects of fluid volume in seawater drowning. Annals of Internal Medicine 1967; 67:68-80
- Modell JH, Davis JH. Electrolyte changes in human drowning victims. Anesthesiology 1969; 30: 414-420
- Modell JH. Current concepts: Drowning. New England Journal of Medicine, 1993; 328(4): 253-256
- Modell JH, Bellefleur M, Davis JH. Drowning without aspiration: is this an appropriate diagnosis?. Journal of Forensic Sciences 1999; 44: 1119-1123
- Morild I. Pleural effusion in drowning. The American Journal of Forensic Medicine and Pathology 1995; 16: 253-256
- Orlowski JP. Drowning, near-drowning, and ice-water submersions. Pediatric Clinics of North America 1987; 34: 75-92
- Peabody AJ. Diatoms and drowning – a review. Medicine, Science and the Law 1980; 20: 254-261
- Pearn J. Drowning and alcohol. Medical Journal of Australia 1984; 141: 6-7
- Pearn J. Pathophysiology of drowning. The Medical Journal of Australia 1985; 142: 586-588
- Polson CJ, Gee DJ. Drowning. Chapter 11. In: ‘The essentials of forensic medicine’, Polson CJ and Gee DJ (3rd Edition), Pergamon Press 1973, Oxford, UK
- Quan L, Cummings P. Characteristics of drowning by different age groups. Injury Prevention 2003; 9: 163-168
- Ramsay DA, Shkrum MJ. Homicidal blunt head trauma, diffuse axonal injury, alcohol intoxication, and cardiorespiratory arrest: a case report of a forensic syndrome of acute brainstem dysfunction. The American Journal of Forensic Medicine and Pathology 1995; 16: 107-114
- Rutty GN. Post-mortem changes and artefacts. Chapter 4. In: ‘Essentials of autopsy practice – Volume 1’, Rutty GN (Ed), Springer-Verlag London Limited 2001, UK
- Saukko P, Knight B. Immersion deaths. Chapter 16. In: ‘Knight’s Forensic Pathology’, 3rd Ed Saukko P, Knight B (Eds), Arnold Publishing 2004, London UK
- Suzuki T. Suffocation and related problems. Forensic Science International 1996; 80: 71-78
- Tipton MJ. The initial responses to cold-water immersion in man. Clinical Science 1989; 77: 581-588
- van Beeck EF, Branche CM, Szpilman D et al. A new definition of drowning: towards documentation and prevention of a global public health problem. Bulletin of the World Health Organisation, Volume 83 Number 11 November 2005
- Wilder-Smith E, Chow A. Water immersion and EMLA cause similar digit skin wrinkling and vasoconstriction. Microvascular Research 2003; 66:68-72
- Wilder-Smith E, Chow A. Water-immersion wrinkling is due to vasoconstriction. Muscle and Nerve 2003; 27:307-311
- Wintemute GJ, Teret SP, Kraus JF, Wright M. Alcohol and drowning: an analysis of contributing factors and a discussion of criteria for case selection. Accident Analysis and Prevention 1990; 22: 291-296
- Wolf S. Sudden death and the oxygen-conserving reflex. The American Heart Journal 1966; 71: 840-841
- Yorulmaz C, Arican N, Afacan I et al. Pleural effusion in bodies recovered from water. Forensic Science International 2003; 136: 16-21



